A Healthcare Leader’s Guide to EHR Implementation
The global health crisis sped up digital transformation in healthcare, with numerous medical organizations (including possibly yours) pushing themselves to adopt electronic health record systems. But in the rush, some skip proper planning, leading to costly mistakes and underused systems. Failure rates for electronic health record system adoption range between 50% and 70% across various healthcare settings.
This article is your guide to avoiding all the standard mistakes these companies make during digital transformation. We’ll examine why EHR implementations fail and share clear strategies for building a successful, long-lasting system that keeps up with the changing healthcare environment.
Content
Switching to a new EHR system is an important step in modernizing medical services, improving patient care, and reducing administrative burdens. However, in practice, EHR projects often encounter difficulties and, in some cases, completely fail to meet specific medical needs. The reasons are usually not technical but organizational and strategic.
In the U.S., satisfaction with recent EHR implementations has declined significantly since 2022. 40% of healthcare leaders reported misses in their recent deployments, while only 38% of other healthcare providers noted that the implementation hit the mark. What’s more, 75% of those dissatisfied continued to report low satisfaction two or more years later.
These statistics may look grim, but they’re completely avoidable. Let’s explore the key factors that can lead to EHR implementation failures and how our team helps you prevent them.
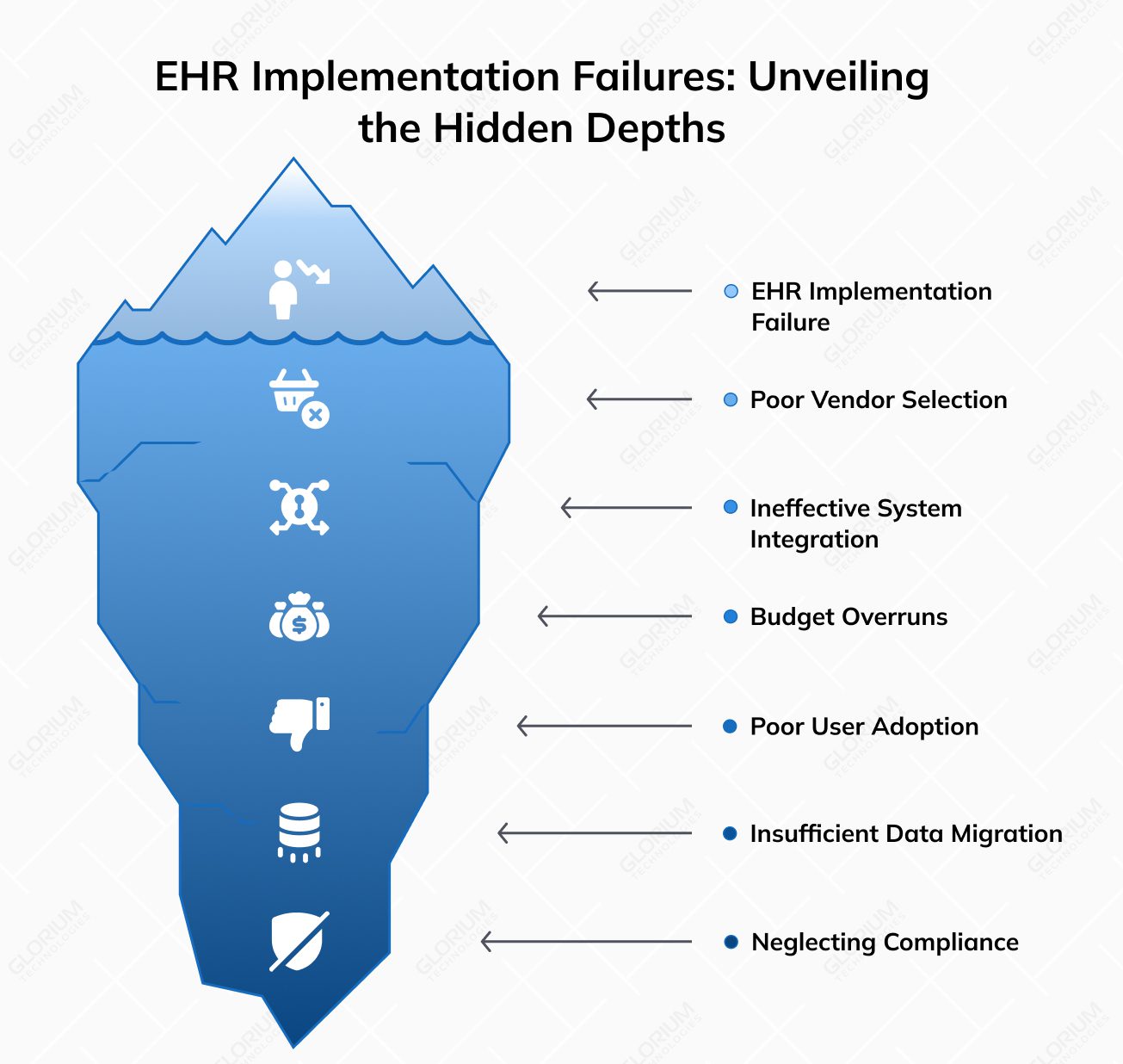
A failed EHR software implementation often begins at the vendor and solution selection stage. In an attempt to save money, some healthcare facilities may settle on solutions with limited functionality or a lack of support, which further complicates the work for in-house teams. The wrong choice of a platform, in turn, leads to incompatibility with existing processes, increases the need for constant refinements, and causes dissatisfaction among end users, including doctors, nurses, and administration.
At Glorium Technologies, we prevent this from happening before the project rollout. We explore your specific healthcare needs and processes at the analysis and audit stage, which gives us a deep understanding of your objectives. Additionally, our expertise in the industry equips us with a profound knowledge of the solutions available so that we can choose the one that fully meets your expectations.
A medical information system operates in the dynamic healthcare environment. EHR software must effectively interact with laboratory systems, hospital management systems, accounting apps, PACS, and other tools. When integration is not thought out or implemented superficially, medical staff are forced to duplicate data, manually transfer information, or work with incomplete patient records. This creates chaos, increases the risk of errors, and leads to a loss of trust in a system.
Our healthcare experts solve this issue by customizing and integrating your EHR with other tools you use, ensuring secure data transfer, real-time updates, and 100% compliance. As a result, you get a system that not only digitizes your paper-based processes but also centralizes your operations and keeps all data in sync.
The financial factor often becomes critical in determining whether EHR software implementation will be successful. When planning the budget, institutions focus mainly on license fees or the initial cost of implementation. Later, however, additional costs may arise. Those are related to data transfer, technical support, additional module implementation, staff training, and adapting a system to real processes.
The lack of realistic financial planning leads to the project either being stopped or constantly going over budget. The solution to this problem is choosing an EHR implementation vendor with transparent pricing and a cost-efficient approach to healthcare software development. Glorium Technologies, for example, provides clients with clear budgeting for each project, eliminating situations when unexpected investments are required.
Another significant reason why EHR implementations may not function properly is that the system doesn’t fit into personnel’s daily workflows. When an EHR solution is implemented without being tailored to the key tasks of doctors and nurses, it inevitably leads to resistance. Staff perceive the system as an additional burden rather than a tool to facilitate work. As a result, the integrated solution is used only partially or ignored altogether.
Glorium Technologies specializes in building user-centered solutions for healthcare. The tools we design and integrate are always intuitive and easy to use. Through early involvement and feedback from doctors, nurses, and administrators, we ensure the system is optimized for the target audience. Our training and support services also help increase staff buy-in and smooth the transition.
Data problems are one of the main reasons why users refuse to work with a new EHR system. When transitioning to EHR platforms, it is important to properly migrate existing patient records. If migration is not planned thoroughly, it can lead to medical and patient data chaos. Outdated, duplicated, or incomplete records are transitioned, which complicates the work of doctors and reduces confidence in the new system.
At Glorium Technologies, we don’t just move data from one environment to another. We carefully clean, structure, and organize it, turning your EHR adoption from a one-time investment into a long-term strategic asset.
The healthcare industry is one of the most regulated markets in terms of patient data processing. EHR system implementation requires strict adherence to security standards such as GDPR, HIPAA, etc. Ignoring these requirements can lead to legal consequences, fines, and an increased risk of sensitive information leakage.
With more than 15 years of experience delivering healthcare solutions, we put security and compliance at the core of our projects. Glorium Technologies ensures that all data protection protocols, including encryption, access control, and audit trails, are integrated into a system. We also stay up-to-date with regulatory changes to ensure that your system remains compliant and secure at all times.
As these pitfalls show, EHR implementation failures are rarely caused by technical issues. More often, they stem from the systemic underestimation of the required digital transformation scale.
To avoid mistakes, the process should be planned comprehensively, involving a detailed analysis of your specific needs, careful vendor selection, a realistic budget, an effective implementation strategy, and attention to users.
Implementing an electronic health record system changes the way healthcare is delivered. An effective system has the potential to reshape internal workflows, streamline interdepartmental collaboration, enhance patient communication, and reinforce regulatory compliance. In fact, the adoption of EHRs has surged across OECD countries, with the number of states reporting over 90% usage in specialist medical offices and hospital emergency care more than doubling between 2016 and 2021.
Still, installing software is not enough. To see meaningful results, your healthcare organization must take a structured, strategic approach to EHR software development and integration. Below, we will explore five key elements that are essential for a successful electronic health record implementation, and without which the system fails or is likely to underperform.
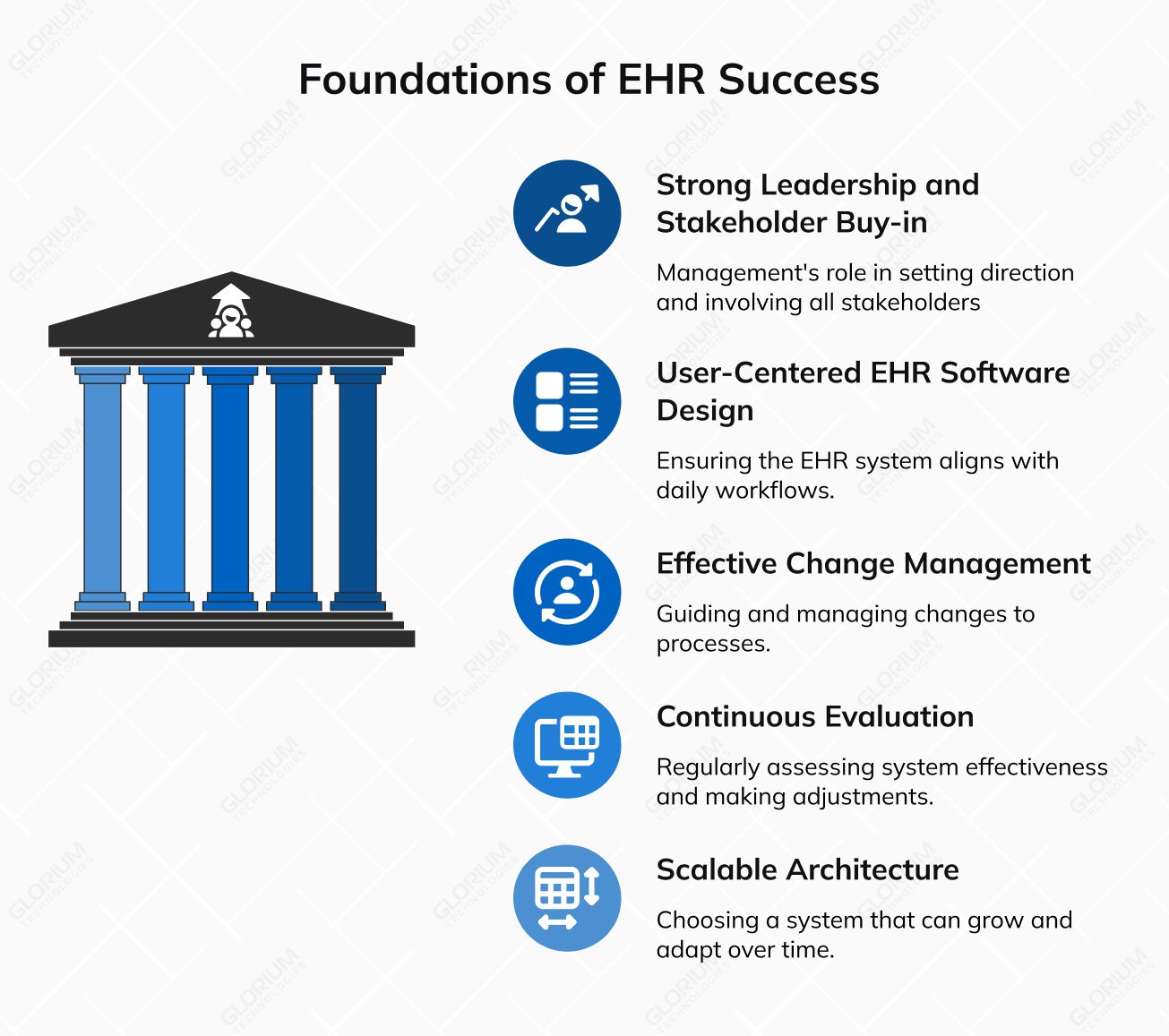
Management’s support is an integral part of the digital transformation process in medicine. The role of your management team is to set strategic direction, provide resources, support internal communication, and actively participate in key decisions. It is also essential to involve all stakeholders (doctors, administrative staff, IT department, etc.) at the early stages of your project. By considering all user groups’ needs before implementing the chosen solution, you will effectively avoid resistance to change.
Adopting a technically advanced but difficult-to-use system is a direct path to implementation sabotage. If medical staff spend more time navigating the interface than exploring patient problems, health information technology is not fulfilling its primary function. So, when considering different EHR systems, pay special attention to the UX/UI design that has to align with the daily workflows of doctors, nurses, and registrars. In practice, this involves:
The transition to digital document management inevitably involves changes to your familiar processes, and changes are often met with user resistance. Your task is to guide and manage these changes rather than simply announce them. It requires a structured approach from you and your staff, which includes the following:
After launching the system, you’ll need to evaluate its effectiveness on a regular basis. This approach allows healthcare organizations to:
Practice shows that medical institutions that have introduced regular monitoring of key indicators (level of use, time spent on record processing, number of system errors, etc.) benefit much more from the adoption of EHRs.
Your needs today may differ significantly from those in 2-3 years. Therefore, from the outset, you should choose a scalable EHR architecture that integrates seamlessly with other healthcare systems, such as laboratory, HR, financial modules, and others.
Flexibility is also essential for adapting to regulatory changes and implementing new functions (such as telemedicine or patient information analytics). Opting for a “closed” or overly rigid system can hinder your institution’s growth and development in the future.
Although the successful implementation of EHR requires time, resources, and patience, the right approach guarantees the result. After all, the best EHR is the one that your staff eagerly uses every day, and this is what you can achieve with expert assistance.
The duration of your EHR implementation will depend on several factors: the scale of your medical institution, the number of users, the complexity of your processes, the level of customization required, and the volume of data migration. For small clinics with simple use cases, a basic implementation can last from 60 to 90 days. This timeline is usually enough for solution adoption, configuration, ongoing training, and fine-tuning.
For medium and large medical institutions, especially those that require deep integration with other systems (for example, practice management systems or financial tools) and the transfer of a large amount of actual patient data, the implementation can stretch for 8-12 months. This includes the stages of technical planning, configuration, system testing, phased launch, and further optimization.
When assessing the project duration, you should also consider the time required to adapt staff to a new system, conduct training, and establish internal processes. High-quality preparation and the phased approach allow you to avoid failures and make the transition as smooth and quick as possible.
Implementing an electronic health record system is a strategic process that requires clear planning, interdisciplinary coordination, and effective change management. Success depends on how effectively a healthcare organization approaches each stage. In this section, you will find a practical step-by-step plan that will help you prepare for the launch of electronic medical records to serve your organization as effectively as you serve your patients.

The first and most important step is to build a strong project team. This should be a cross-functional group that includes clinical, administrative, IT, and financial representatives. If you don’t have internal IT expertise, bring in external experts, such as EHR consultants or software implementation partners with healthcare experience. A strong team will help you choose between various EHR systems and avoid technical and procedural pitfalls at all stages.
At Glorium Technologies, we specialize in delivering customized EHR implementation solutions for healthcare providers. Our team ensures seamless integration, minimizes disruptions, and guarantees a smooth transition from start to finish. With our help, you’re not just implementing EHR systems; you’re setting up your organization for long-term success.
The next step is to create a clear project plan. Together with the selected vendor, define the scope of the implementation, the budget, and an indicative project schedule. This will allow you to stay focused on key objectives and allocate resources effectively.
Before you begin implementation, your vendor will analyze your current IT infrastructure to determine if you have enough server capacity, workstations, network coverage, and backup to support EHR. By leveraging expertise in healthcare software product development, your EHR implementation partner will help you ensure that your current IT infrastructure can handle the load effectively.
Digitization shouldn’t simply duplicate old paper records. Instead, you should audit your existing workflows (both clinical and administrative) and determine what needs to be optimized or automated. For instance, patient registration, transitions between doctors, and appointment scheduling can be streamlined, documented, and seamlessly integrated into an EHR system.
If you take care of the processes before they go digital, you ensure that the system enhances efficiency, reduces errors, and aligns with real-world operational needs. Look for a partner that can guarantee that this process unfolds with zero disruption to your workflows and operations.
The quality of data inputs is a critical aspect of EHR or EMR implementation. Review and clean up existing data: remove duplicates, standardize titles, and ensure completeness of fields. It is important to have a clear plan for data migration. Involve your EHR implementation company to define what data needs to be migrated, in what form, who is responsible for this, and how the post-migration review will be conducted.
Consider onboarding and user training in advance. Doctors need to be able to quickly enter clinical data, nurses need to easily update appointments, and registrars should effectively use registration modules. Involve your staff in user acceptance testing before the system goes live to reduce resistance to change and identify problems early.
Once training is complete, conduct a phased rollout, starting with a basic EHR system or module. This will allow you to test system stability, quickly identify issues, and adjust the configuration if necessary. Your system’s launch should be facilitated by ongoing support of your EHR implementation partner in the first weeks after launch, helping your staff adapt.
After launch, it is necessary to implement a result evaluation system to figure out which performance indicators improved, how the level of patient satisfaction has changed, etc. Establish feedback collection channels, such as anonymous surveys, interviews, or technical reports, to gather insights on the basic EHR functions and their impact on how your staff works.
Altogether, these clear, structured steps will help your team avoid common mistakes, improve the quality of healthcare delivery, and lay the foundation for further digital transformation.
In this section, we will outline the key roles and responsibilities that your partnering team must take to successfully fulfill their mission and support your organization’s goals.
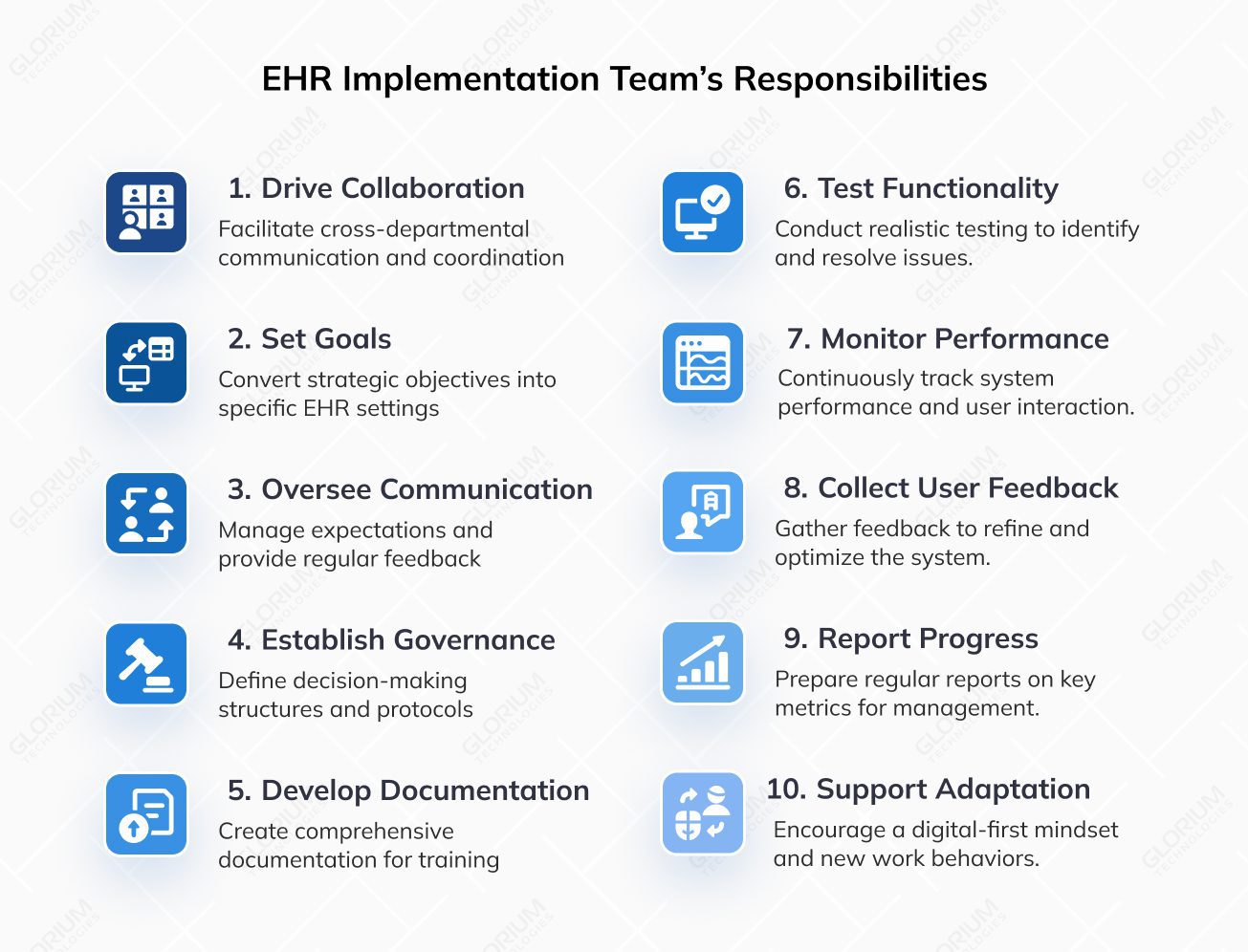
The EHR implementation project manager should help medical, administrative, IT, and finance departments collaborate closely. This coordination ensures that all EHR users understand the project’s goals, resources, and timelines. Effective communication allows for quick and informed decisions that take into account the needs of different departments.
The team should analyze strategic goals (for example, improving service quality, reducing documentation time, reducing errors) and translate them into specific EHR settings: record templates, permission levels, process automation, etc. By doing so, they ensure that your digital platform meets the real business requirements.
The role of your partnering company involves managing expectations, providing regular updates on the implementation status, resolving issues, and indirectly assisting with staff engagement. The communications lead will coordinate information exchanges between the team, management, and external partners, including the EHR vendor.
Effective implementation requires a well-defined decision-making structure. Your EHR implementation team must establish control mechanisms, defining who approves changes, outlining the decision-making process, detailing the testing and trial phases, and setting up feedback and escalation protocols for managing risks or failures.
Documentation is a fundamental part of every EHR project. The EHR implementation team is responsible for creating and maintaining a structure: process descriptions, technical specifications, user guides, records of decisions made, and test results. Once launched, this documentation becomes the basis for user training, support, and future updates.
Your partnering company should conduct testing under conditions that closely mirror real-world use cases, such as working with medical records, compiling medical histories, and sharing data between departments. This stage helps identify configuration errors, interface issues, and areas for process improvement.
After launch, continuous monitoring is crucial, including tracking module load times, recording data entry speed, and usage of essential functions. It’s equally important to evaluate staff sentiment, the tool adoption speed, user feedback, and staff requests for extra features or modifications. This ongoing oversight ensures high-quality performance and helps gauge the EHR system’s real-world impact.
Regular collection of user feedback through surveys, technical reports, and focus groups empowers your team to refine system configurations. Your partnering company should aid you in this process and incorporate the insights into further project phases. By optimizing workflows, adding features, and adjusting the system to the needs of healthcare professionals, you will ensure the system aligns with user expectations.
Your EHR implementation team should regularly prepare comprehensive reports for management, focusing on key metrics such as active user count, average record entry time, error rates, staff satisfaction, and interdepartmental collaboration. A transparent reporting approach enables informed decision-making and strategic course corrections when necessary.
A vital responsibility of your partnering team is to provide ongoing maintenance and support for cultural change, encouraging a digital-first mindset, motivating employees to embrace the EHR system, and fostering new work behaviors. This process addresses not only the technical aspects but also the psychological and organizational challenges that come with digital transformation.
As the amount of medical data grows, effective information management is becoming more and more important for success. It’s no longer the question of “if” we should use an electronic health record system; it’s the question of “when” and “how.” Organizations that put off this process or don’t have a clear plan risk falling behind in both operational efficiency and how their patients see them.
To avoid this, medical facilities should treat EHR system implementation strategically. EHR is not just software but the cornerstone of your healthcare institution’s digital future that enhances the quality of care, improves transparency in management processes, and strengthens your resilience in the face of future challenges.
Schedule a consultation with experts who truly understand the complexities of healthcare environments and get the solution that frees you from inefficiencies.
An EHR implementation specialist coordinates the entire process, from technical preparation to staff training. They adapt a system to your institution’s specific needs, monitor compliance and deadlines, ensure integration testing, and guarantee a smooth transition from a legacy system. It is better to involve this specialist at the planning stage, before choosing a platform or provider.
Preparation starts with clear communication. You should clearly communicate the implementation goals and benefits for each role. Next, provide training sessions tailored to the specific user roles (doctors, nurses, registrars, etc.). It’s also essential to offer real-time support during the launch phase (for example, an internal chat or an on-call coordinator) to ensure quick issue resolution and maintain user confidence in the crucial first weeks.
Both quantitative and qualitative metrics are essential for assessing the success of your electronic health record (EHR) implementation. Key metrics include:
Additionally, it’s important to evaluate whether an EHR or EMR system complies with legal and security standards to ensure data protection and regulatory adherence.
The duration depends on the scale of the institution, the complexity of processes, the volume of data migration, and the chosen platform. On average, a basic implementation takes from 60 to 90 days for a small clinic and up to 6-12 months for large hospitals. This includes project evaluation and planning, configuration, integration, EHR training for your staff, and system launch.