Overcoming 5 Key Hospital Revenue Cycle Management Challenges
Consistent and organized finance management is vital to any hospital or medical organization. Incoming payments, claims processing and reimbursement, margins, and other transactions are a daily part of hospital management, and executives are always looking for ways to improve this process.
Revenue cycle management is a complex, but manageable process that can be enhanced through benchmarking and automation.
Content
For a profitable and efficient healthcare practice, smooth revenue cycle management is vital. Anyone who has ever dealt with finances in healthcare knows that denied claims or billing errors can result in huge revenue losses, let alone frustrated clinicians and patients.
In revenue management, mistakes can happen at different stages and at different scales, so there’s always room for improvement when it comes to financial operations.
Healthcare providers are focusing on RCM optimizations to get a more consistent revenue management process, reduce claims, and scale operations. Today a consistent and automated approach to revenue cycle management becomes even more important for a variety of reasons.
Firstly, there is a growing number of points of contact used to process a single payment: hospitals must interact with several payment channels to finalize their transactions.
Secondly, changing health policies, insurance regulations, health plans, and eligibility requirements are all contributing to making revenue cycle management more complicated.
Some healthcare industry trends are making an impact as well, like a shift to value-based care and more patients willing to manage their own health and consequently pay for the care they receive.
All these factors push revenue cycle managers and executives to find and implement long-term strategies for successful hospital RCM.
Let’s take a closer look at the key challenges that are hindering seamless revenue cycle management in most healthcare organizations.
Depending on the hospital, challenges can be very different from case to case. While one institution may struggle to automate payment collection and billing processes, another can find managing denied claims a real issue.
We will address some of the most common revenue cycle management challenges that any hospital can face at a certain stage.
Collecting payments before services are received is a major part of the revenue cycle and the one where issues can happen quite often. The tricky part of this stage is that many patients can’t afford or are not willing to pay the whole amount in advance, which creates a need to manage debts.
In fact, around 48% of patients are not able to pay their entire medical bill upfront. At the same time, clinicians try to not press patients to pay upfront, which could cause them to migrate to another health provider.

One way to resolve the issue with the inability to pay upfront is to provide patients with price estimates. Additionally, 38% of patients said that having a payment plan option would increase their chances to pay bills on time.
Another challenge with billing is the collection of patient responsibilities before the service is received. Additionally, the number of prior authorizations is only growing with time, which means the staff needs to process insurance eligibility and other requirements before obtaining the payment.
It is a complex process that sometimes involves many stages of document validation. Hospitals need to focus on setting up an automated, streamlined and integrated process to collect payments and eliminate billing errors.
Accounts receivable involves debt payments, denied claims, and all the other payments that patients owe to their healthcare provider. Poor monitoring and tracking of the A/R process result in tremendous revenue losses for hospitals.
Claims processing is a separate branch of hospital revenue management that can produce big financial damages when neglected. Mostly, issues happen when patients deny a claim for a reason that the hospital management system cannot identify.
Considering that nearly one-third of hospitals in the US are managing claims manually, this can be a common bottleneck in hospital revenue cycle management.
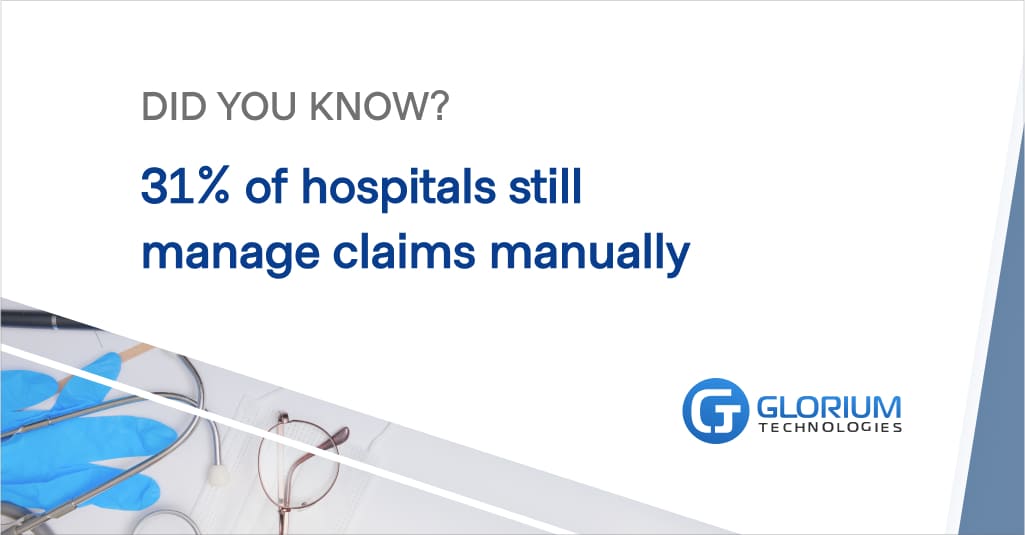
According to McKinsey, around 70% of claims management can be automated. Automating claims management can help define the root of the error, alert administrators where the denial occurred, and significantly reduce the costs of the problem.
One of the biggest challenges with the hospital revenue cycle management is the never-ending discrepancy between the front-end and back-end parts of the cycle. The front-end part involves the patient and often medical staff, who collect patient data and receive the payment.
The problem is that the people handling those primary stages of the revenue cycle don’t have a comprehensive knowledge of what the process looks like further down the line, on the back-end, when the payment needs to be transitioned into an insurance claim.
Because of this lack of understanding of the whole picture, hospital staff can’t identify whether the issue has occurred.
To increase staff awareness of the actual process of revenue cycle management, executives have to provide regular educational training.
While the revenue cycle management is far from perfect in many cases, there are still many ways to improve the flow.
After exploring a few major challenges that medical practice leaders often face, it’s safe to say that the key to improvement lies in proper data monitoring, staff training, and the use of sophisticated RCM software for automation.
While it can be complicated to integrate a revenue cycle management system and dedicate costs and resources to train staff, financial management is a branch of healthcare that can’t be neglected.
There are many solutions to help healthcare providers ease the current challenges in hospital revenue management.
To ensure accurate and seamless reimbursement, it is crucial to first identify the gaps and find the blind spots in the cycle. Obviously, this can’t happen without thorough monitoring and data benchmarking.
This first step will give organizations a complete picture of their revenue cycle management and help prioritize areas for improvement.
Additionally, measuring KPIs based on the acquired information will help define and avoid emerging issues. The Healthcare Financial Management Association (HFMA) recommends focusing on these 5 KPIs:
Collecting accurate clinical and financial data will equip the foundation for frictionless transactions going forward.
At the first step of the educational process, every staff member should know not only what lies within their role, but how this role fits in the overall revenue cycle.
A complete understanding of how the system functions as a whole will help increase responsibility and accountability among staff members and reduce manual errors.
While educating medical personnel is important, it is equally critical to establish firm financial policies for the patients. Despite the fact that patient financial responsibility has been steadily growing over the last few years, many people still find it challenging to pay upfront and manage bills on their own.
It may seem an appealing decision to let patients pay later in order to keep them, but this is a short-term strategy that hinders the revenue cycle for any hospital.
To reduce the number of late payments and debts, hospitals should implement convenient pre-service payment options, provide price estimates, and offer credit card-on-file payments.
There are too many areas of revenue cycle management that need automation and advanced monitoring, and the best way to enhance the process is to implement a hospital revenue cycle management software system.
Despite the intensified digitalization of the healthcare industry, there is still only a small percentage of health plans that include digital payments. However, automation of this part of the cycle can significantly reduce hospital expenses.
Sophisticated hospital RCM software can also properly manage claims processing and denial, automate payment conversion, improve data collection, monitor patient responsibility and help manage exceptions.
Overall, software shortens the revenue cycle for the hospital and helps maximize net income without repelling patients. Here are a few of the essential features of hospital RCM software:
Before investing in the development of a custom solution, make sure that the software provider has proper certifications and expertise in the healthcare sector. Additionally, the RCM should easily integrate with other software systems that are used by the hospital.
With more than 10 years of industry knowledge, Glorium helps start-ups swiftly reach the market with excellent service and custom solutions. We can build a custom hospital RCM from scratch or enhance your existing system.
Learn more about our healthcare software development solutions today!