EDI in Healthcare: How to Maximize Your Efficiency



It’s surprising that many healthcare organizations are still clinging to the old-school method of managing patient records with piles of paper. Not only does this seem like a relic from the past, but it also drains precious time and resources that could be better spent on patient care.
Up to 50% of US hospitals nowadays are facing a potential obstacle to improving healthcare coordination-the increase in unorganized data that could hinder connected care efforts. The good news is there’s a reliable solution to help hospitals overcome these challenges.
Healthcare EDI transactions provide a simple and efficient way to automate various healthcare tasks, such as billing, enrollment, checking eligibility, and managing referrals. EDI in healthcare offers a glimpse into an efficient future for healthcare organizations, but what steps do they need to take in order to make this vision reality?
Content
EDI, or Electronic Data Interchange, plays a pivotal role in the healthcare industry by enabling healthcare providers to exchange critical data in a standardized and secure manner.
According to a recent ONC Interoperability study, a significant 88% of hospitals are actively engaging in health data exchange efforts. However, these hospitals encounter substantial challenges in effectively leveraging public health data due to the variability in their information systems and the absence of standardized data practices.
At its core, EDI in healthcare relies on the ANSI X12 (American National Standards Institute X12) and HIPAA (Health Insurance Portability and Accountability Act) standards, which establish a standardized format for data exchange while ensuring the utmost protection of patient privacy.
This standardized approach serves as a common language for the seamless exchange of sensitive healthcare information among various systems and healthcare entities.
Healthcare providers, insurance agencies, and other entities are utilizing healthcare EDI to facilitate efficient communication of data. Through this exchange, a variety of documents such as claims, status inquiries, and payment information can be submitted quickly and with precision using retail pharmacy claim transaction sets.
The ability for organizations to submit these types of healthcare EDI transactions is driving growth within the global healthcare EDI market, along with advances in technology enabling rapid transmission speeds when submitting group premium payments or health plans.
Software solutions provided by specialists familiar with ithe healthcare industry needs guarantee correct implementation that will ensure consistent results across different stakeholders involved within the sector, including employers handling compensation details.
The Health Insurance Portability and Accountability Act (HIPAA) is a federal law enacted in 1996 to protect patient privacy and secure medical data. If you want to learn more about HIPAA, we have a detailed explanation about the Healthcare Personal Data Protection Act.
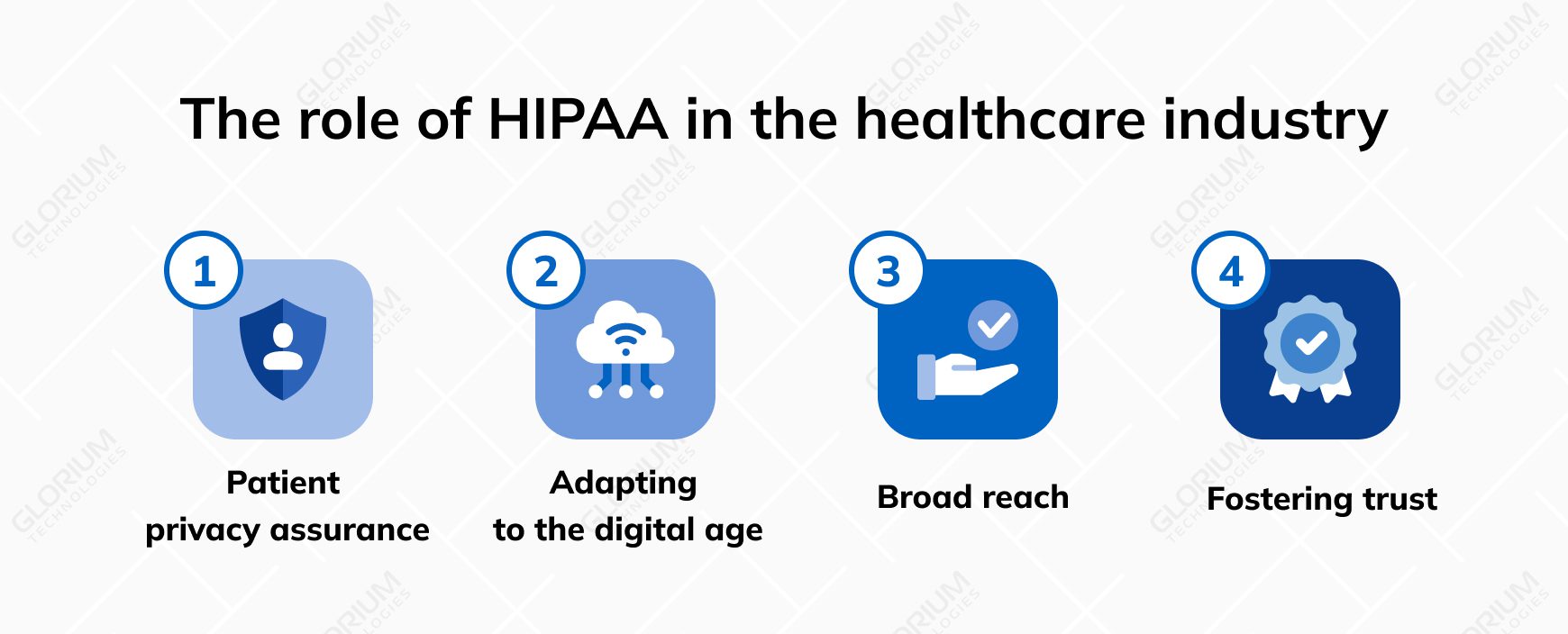
HIPAA is critically important for several reasons:
HIPAA mandates standardized electronic health care transactions, including the ANSI X12-formatted EDI functional validation transaction that ensures secure and reliable data exchange.
Let’s explore the numerous advantages of implementing EDI, from streamlining communication to enhancing patient care and outcomes.
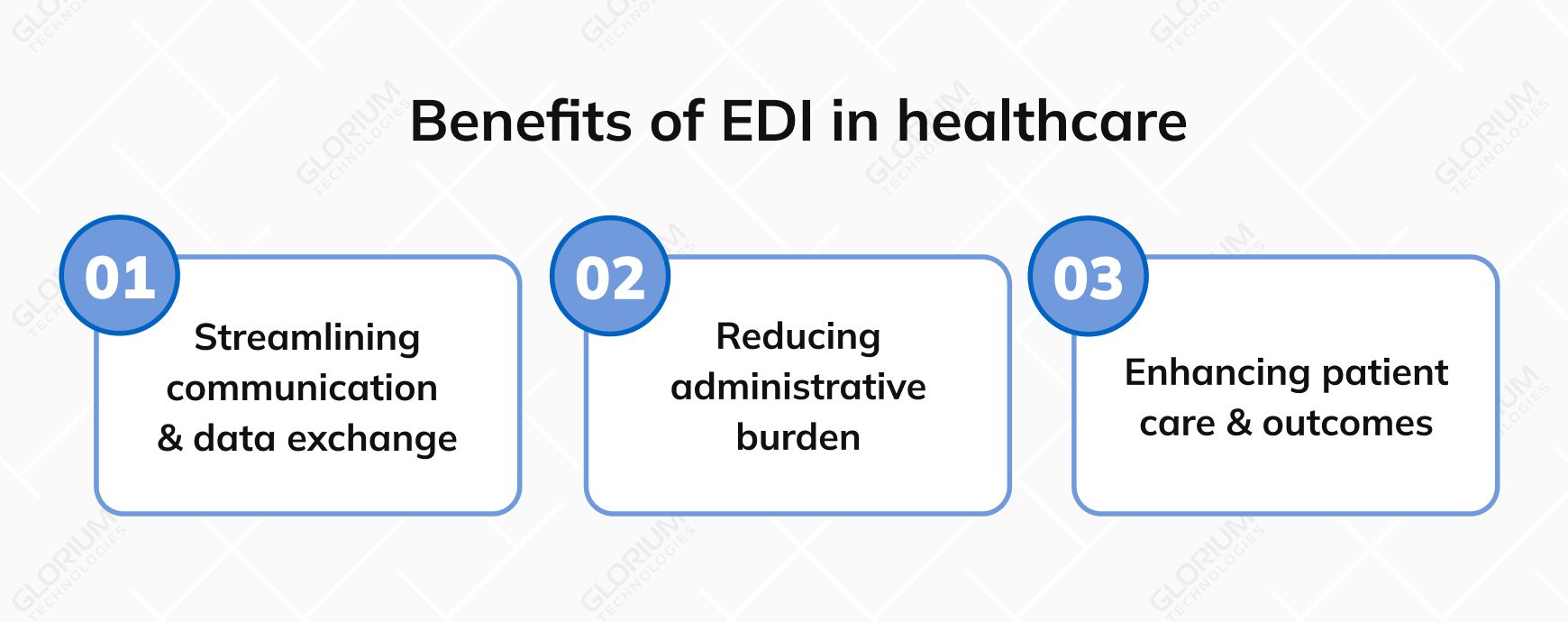
Imagine a world where providers can seamlessly transmit comprehensive health care claim information electronically, including patient demographics, diagnosis codes, procedures, and charges – all in a matter of moments. This is the power of EDI, specifically the EDI 837 transaction.
By replacing tedious manual paperwork, healthcare EDI eliminates the risk of errors or missing data, making medical transactions more efficient and accurate.
It’s not just about speed; it’s about precision. Healthcare education also benefits from automation, simplifying collaboration with payers. With streamlined communication, providers can quickly discuss health care claim statuses, request additional information, and resolve discrepancies.
EDI solutions aren’t just efficient; they’re cost-effective too. Manual transactions can cost as much as $4.92 per transaction, whereas EDI transactions typically come at a fraction of that cost – just $0.67 per transaction, as of 2022.
Integrating EDI into your Enterprise Resource Planning (ERP) system further enhances efficiency, leading to cost savings, time optimization, and improved patient care outcomes. It’s not just about reducing administrative burdens; it’s about transforming healthcare operations for the better.
EDI isn’t just about paperwork and cost savings; it’s about elevating patient care and outcomes. By facilitating seamless communication between providers, patients, and other participants in the system, EDI ensures that data is not only transmitted quickly but also accurately.
This precision in EDI transactions supports a more reliable approach to health-related communications, saving valuable time in claims submission and adjudication tasks. Swift transactions of information to multiple parties optimize performance output and minimize rejections, reducing the need for rework.
Embarking on the journey of healthcare EDI implementation can be immensely beneficial, but it comes with its share of challenges. Let’s delve into these hurdles and explore effective solutions, ensuring seamless integration, compliance with regulations, and robust data security.
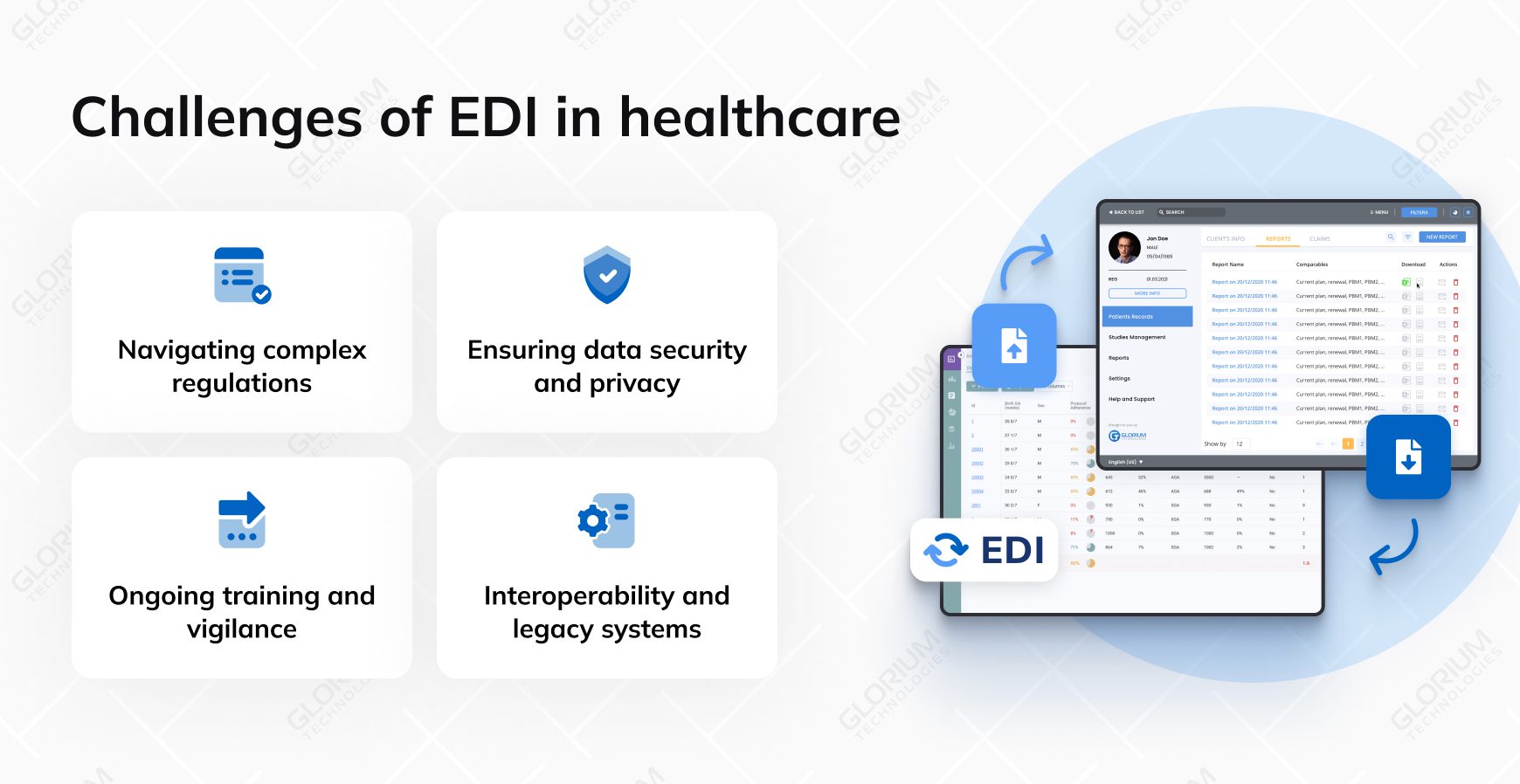
Organizations must navigate a complex web of regulations, particularly those outlined in the Health Insurance Portability and Accountability Act (HIPAA) and Administrative Simplification rules. These regulations mandate stringent requirements for EDI transactions, making compliance a formidable challenge. Staying updated with evolving ASC X12 protocols under HIPAA’s Electronic Data Interchange Rule is essential.
Assemble a dedicated team with programming expertise and an intricate understanding of HIPAA requirements. This team should continuously monitor updates to ensure compliance. By doing so, you build a strong foundation for successful EDI implementation while meeting the healthcare industry standards.
Challenge: Protecting sensitive patient data during EDI transactions is paramount. Data breaches are a common concern, and maintaining the highest security standards is imperative. Healthcare organizations need to establish privacy protocols, conduct regular risk assessments, and keep audit trails up-to-date to swiftly address potential risks.
Implement comprehensive security measures to safeguard electronic exchanges. This includes encrypting data, establishing robust privacy protocols, and conducting thorough risk assessments. Collaborate with service providers who specialize in cybersecurity to fortify your defenses against cybercriminals’ efforts to access private information.
Challenge: Ongoing training is crucial, especially for employees who handle confidential data and access systems vulnerable to cyber threats. Keeping up with evolving cybersecurity protocols and maintaining a proactive stance against potential threats can be challenging.
Regularly conduct training sessions to educate employees about security procedures and best practices. These sessions should emphasize the importance of adhering to established protocols to safeguard digital assets, whether it’s personally identifiable data or corporate financial records. By continually revising plans and staying updated with the latest cybersecurity developments, your organization can maintain a robust defense posture.
Many healthcare organizations grapple with the challenge of integrating EDI seamlessly into their existing IT infrastructures, which often include legacy systems. These legacy systems may not be inherently compatible with modern EDI solutions, leading to potential disruptions or data degradation during implementation.
To address this challenge, healthcare organizations should invest in EDI solutions that offer robust integration capabilities. This may involve customizing EDI software to work harmoniously with legacy systems or gradually phasing out outdated systems in favor of more interoperable solutions. A carefully planned integration strategy ensures that EDI implementation enhances, rather than disrupts, existing workflows and data management processes.
From claims processing and pharmacy management to eligibility verification and secure payment processing, healthcare EDI solutions have redefined efficiency, accuracy, and patient care coordination.
In this exploration, let’s look at the top five types of healthcare EDI solutions, shedding light on their pivotal roles in streamlining operations, reducing administrative burdens, and ultimately contributing to the delivery of higher quality healthcare services.
Claims processing EDI is a cornerstone for providers, streamlining the submission and processing of healthcare claims. This solution enables providers to electronically submit claims to insurance companies, reducing paperwork and expediting reimbursement processes.
The automation of claims processing ensures the accuracy and efficiency of claims adjudication, benefiting both providers and payers.
Pharmacy EDI solutions play a pivotal role in enhancing patient safety and medication management. These solutions facilitate the electronic exchange of prescription and medication-related information between pharmacies and providers. This electronic data interchange expedites medication order processing and prescription refills, contributing to better patient care coordination and reducing the risk of medication errors.
Healthcare payments EDI solutions streamline financial transactions within the healthcare sector. They enable secure electronic payment processing for services rendered, including insurance premiums, medical bills, and reimbursements.
By replacing manual payment processing and paper-based transactions, healthcare payments EDI reduces administrative costs and simplifies financial transactions.
Eligibility and benefit verification EDI solutions are vital for revenue cycle management in healthcare. They allow providers to verify patients’ insurance eligibility in real-time, ensuring active coverage.
Additionally, this type of healthcare EDI helps providers determine co-pays and deductibles upfront, leading to more accurate revenue estimation and reducing financial surprises for patients.
Lab results and diagnostic reports EDI streamline the electronic exchange of critical medical test data between laboratories and healthcare providers. This technology enhances the speed and accuracy of diagnosis and treatment decisions. It fosters efficient communication among laboratories, healthcare providers, and patients, ultimately improving patient care outcomes and diagnostic precision.
These five types of healthcare EDI solutions play a crucial role in streamlining healthcare operations, reducing administrative burdens, and improving patient care by ensuring the efficient exchange of critical healthcare information.
Achieving a seamless EDI (Electronic Data Interchange) implementation in healthcare demands a strategic approach, careful software selection, clear communication channels, and robust staff training. Let’s dive into the best practices that healthcare organizations can follow to harness the full potential of healthcare EDI while avoiding common pitfalls.

The first step in a successful EDI journey is selecting the right software solution tailored to healthcare needs.
When evaluating healthcare EDI software options, consider factors such as customization capabilities, cost-efficiency, user-friendliness, and customer support. Ensure that the chosen solution provides robust security guarantees, compatibility with existing infrastructures, and automation of transactions for standardized communication. Scalability is vital to accommodate future growth without the need to switch providers.
Transparent communication is key to a successful EDI implementation, as it involves multiple stakeholders.
Foster a culture of transparency and collaboration within your healthcare organization. Provide training on effective communication methods to ensure all parties understand their roles in the healthcare EDI process. This transparency promotes patient welfare, regulatory compliance, trust, and accountability among healthcare professionals.
Providing staff training and support
Maximizing the benefits of EDI requires skilled and confident staff members who can navigate the system effectively.
Invest in training initiatives for your healthcare staff. Offer comprehensive instruction and ongoing support to ensure they are proficient in using EDI systems. Create a culture of continuous learning and clearly define incentives for staff who excel in EDI adoption. Engage employees in the implementation process and ensure user interfaces are intuitive and user-friendly.
Electronic Data Interchange (EDI) in the healthcare industry represents a pivotal shift in how data is exchanged within the medical field. It entails the electronic exchange of standardized business documents, such as medical claims, patient records, and billing information, among healthcare providers, insurers, and various stakeholders. EDI brings forth a digital transformation by replacing traditional paper-based processes with secure electronic EDI transactions, revolutionizing communication in the healthcare sector.
The advantages of implementing EDI in the healthcare industry are multifaceted. First and foremost, it introduces unparalleled efficiency by reducing the need for manual data entry and cumbersome paperwork. Moreover, EDI significantly contributes to cost savings as automation decreases transaction-related expenses. This not only benefits healthcare providers but also payers, fostering a more cost-effective healthcare system.
In addition, EDI ensures data accuracy, mitigating the risk of errors and discrepancies in patient records and claims. This accuracy translates to improved patient care, as healthcare providers gain rapid access to precise information, enabling them to make more informed decisions for better patient outcomes.
The adoption of Electronic Data Interchange in healthcare does not come without its challenges. Compliance with complex healthcare regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), is imperative to protect patient data during EDI transactions.
Data security remains a top priority in the healthcare industry, necessitating stringent measures to safeguard sensitive patient information and thwart data breaches.
Additionally, integrating EDI with existing legacy systems can pose compatibility issues for healthcare organizations. Overcoming these challenges is essential to fully unlock the potential of Electronic Data Interchange.
Despite these challenges, EDI is on the rise in the healthcare sector. As technology continues to advance and healthcare organizations adapt to the digital era, EDI is positioned as a game-changer in the near future. EDI promises even greater efficiency and innovation, further solidifying its role as a cornerstone of modern healthcare operations.
Glorium Technologies specializes in crafting custom EDI software for healthcare organizations. With a deep industry understanding and a commitment to excellence, we create EDI solutions that optimize data exchange, streamline operations, and ensure compliance with regulations like HIPAA.
An example of EDI in healthcare is when a medical provider uses EDI to send an inquiry by providing data like the member ID number and date of birth.
EDI, which stands for Electronic Data Interchange, is a system employed by healthcare providers to facilitate the secure exchange of data using standardized formatting. This ensures that information can be accurately exchanged between healthcare organizations with ease.
EDI in healthcare serves as a versatile tool for the automated transfer of various types of data critical to healthcare operations. It streamlines the submission and processing of insurance claims, facilitates efficient communication between providers and pharmacies for prescription data and medication orders, and enables secure electronic financial transactions for services like insurance premiums and medical bills.
Additionally, it verifies patients’ insurance eligibility in real-time, facilitates the electronic exchange of vital medical test data, and securely maintains patient health records while adhering to privacy regulations such as HIPAA.
Overall, EDI in healthcare is a dynamic solution that enhances patient care, reduces administrative burdens, and improves operational efficiency throughout the healthcare industry.
HIPAA (Health Insurance Portability and Accountability Act) standards for EDI in healthcare specify the use of the X12N protocol and the utilization of ASC X12 Version 5010 (HIPAA 5010) codesets when transmitting electronic data.
EDI plays a crucial role in simplifying electronic data interchange, particularly, the submission of retail pharmacy claims in the healthcare sector. Instead of relying on traditional paper-based methods, healthcare providers and pharmacies can utilize EDI systems to electronically submit and process retail pharmacy claims efficiently.
With EDI, it becomes easy to submit retail pharmacy claims, ensuring accurate and timely reimbursements while enhancing the overall efficiency of healthcare operations.